Parkinson’s Disease – Physiotherapy Management.
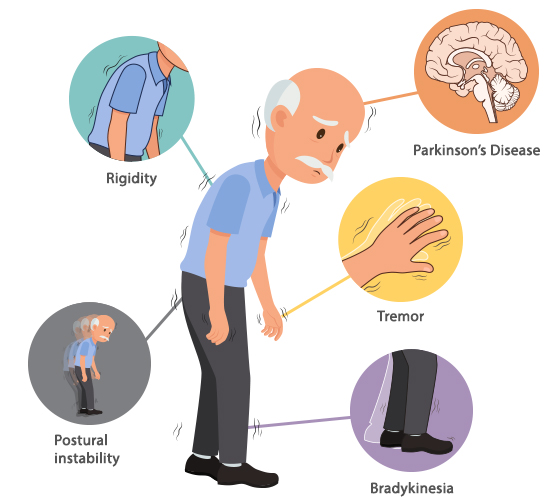
Parkinson’s Disease is a neurodegenerative brain disorder that progresses slowly in most
people. Symptoms can take years to develop, and most people live for many years with
the disease. The symptoms caused by Parkinson’s include an ongoing loss of motor
control (resting tremors, stiffness, slow movement, postural instability) as well as a
wide range of non-motor symptoms (such as depression, loss of sense of smell, gastric
problems, cognitive changes and many others).
Although Parkinson’s Disease is not fatal, the complications caused
by Parkinson’s are a leading cause of death. The average age
of diagnosis is around 60, but approximately 15% of people with Parkinson’s Disease are
diagnosed before age 50 and are said to have young-onset Parkinson’s disease.
What is Parkinsonism?
Parkinsonism is a general term that refers to a group of neurological disorders that
cause movement problems similar to those seen in Parkinson’s Disease, such as
tremors, slow movement, and stiffness. Under the category of Parkinsonism, there are a
number of disorders, some of which have yet to be clearly defined or named. Early in the
disease process, it is often hard to know whether a person has idiopathic (meaning “of
unknown origins”) Parkinson’s Disease or a syndrome that mimics it. Parkinsonisms, also
known as atypical Parkinson’s Disease or Parkinson’s plus, represent about 10% of all
diagnosed cases of Parkinsonism (about 100,000 individuals). They tend to progress
more rapidly than Parkinson’s, present with additional symptoms such as early falling,
dementia or hallucinations, and do not respond or respond only for a short time to
levodopa therapy.
Following are descriptions of some of the most common Parkinson’s plus disorders.
It is important to remember that many people will not exhibit the cardinal symptoms
necessary for a diagnosis of a specific disorder and will simply be labelled “Parkinsonism.”
Drug-Induced Parkinsonism can be difficult to distinguish from Parkinson’s, though
the tremors and postural instability may be less severe. It is usually the side effect of
drugs that affect dopamine levels in the brain, such as antipsychotics, some calcium
channel blockers and stimulants like amphetamines and cocaine. If the affected
person stops taking the drug(s), symptoms usually subside over time but may take as
long as 18 months to do so.
Progressive Supranuclear Palsy (PSP) is slightly more common than ALS (also
called Lou Gehrig disease). Symptoms usually begin in the early 60s. Common early
symptoms include forgetfulness, personality changes, and loss of balance while
walking that results in unexplained falls. The visual problems associated with PSP
generally occur three to five years after the walking problems and involve the inability
to aim the eyes properly because of weakness or paralysis of the muscles that move
the eyeballs. Individuals with PSP may have some response to dopaminergic treatment
but may require higher doses than patients with Parkinson’s disease.
Multiple System Atrophy (MSA) (also referred to as Shy-Drager syndrome) is the
term for a group of disorders in which one or more systems in the body stop working.
In MSA, the autonomic nervous system is often severely affected early in the course of
the disease. Symptoms include bladder problems resulting in urgency, hesitancy or
incontinence and orthostatic hypotension (nOH). In nOH, the blood pressure drops so
low when standing that fainting or near fainting can occur. When lying down, the
person’s blood pressure can be quite high. For men, the earliest sign may be a loss of
erectile function. Other symptoms that may develop include impaired speech,
difficulties with breathing and swallowing and inability to sweat. Like the other
Parkinsonisms, MSA symptoms either don’t respond very much or don’t respond at all
to Parkinson’s medications.
Vascular Parkinsonism is usually caused by clotting in the brain from multiple small
strokes. People with vascular Parkinsonism tend to have more problems with gait than
tremor and have more problems in the lower body. The disorder progresses very
slowly in comparison to other types of Parkinsonism. People might report an abrupt
onset of symptoms or step-wise deterioration (symptoms get worse then plateau for a
while). Symptoms of vascular Parkinsonism may or may not respond to levodopa.
Dementia with Lewy bodies (DLB) is second only to Alzheimer’s as the most common
cause of dementia in the elderly. It causes progressive intellectual and functional
deterioration. In addition to the signs and symptoms of Parkinson’s disease, people
with DLB tend to have frequent changes in thinking ability, level of attention or
alertness and visual hallucinations. They usually do not have a tremor or have only a
slight tremor. The Parkinsonian symptoms may or may not respond to levodopa.
Corticobasal degeneration (CBD) is the least common atypical Parkinsonism. It
usually develops after age 60. Symptoms include a loss of function on one side of the
body, involuntary and jerky movements of a limb and speech problems. It may become
difficult or impossible to use the affected limb, although there is no weakness or
sensory loss. The individual may feel as if the limb is not under his/her voluntary
control. There is no specific treatment at this time for CBD.
Diagnosis of Parkinson’s Disease
There is no definitive test to detect Parkinson’s disease or Parkinsonism. For diagnosis,
doctors take a thorough medical history and may request a number of movement tests.
Because of the observational nature of the diagnosis, Parkinson’s can sometimes be
confused with Parkinsonism, and the diagnosis may need to be revised over time-based
on a speed of disease progression, response to medications and other factors. All the
Parkinsonisms have a loss of dopamine, so a DatScan cannot be used to differentiate
between them and idiopathic Parkinson’s disease.
Treatment of Parkinson’s Disease
There is overlap in treatment for Parkinson’s and Parkinsonisms. Dopaminergic therapy
(the first line treatment for Parkinson’s) can be effective in some Parkinsonisms. Other
common treatments for both Parkinson’s and Parkinsonisms include physical therapy,
occupational therapy and speech therapy; antidepressants and botulinum toxin (Botox) for
dystonia. For all the conditions, healthcare providers aim to treat the symptoms that
most affect a person’s quality of life.
What should I do next?
If you or a loved one is unsure if you have Parkinson’s disease or a form of Parkinsonism,
make an appointment with a movement disorders specialist (MDS). An MDS is a
neurologist who has completed specialized training in Parkinson’s disease and other
movement disorders including the Parkinsonisms discussed in this article.








Leave a Reply