Chronic obstructive pulmonary disease
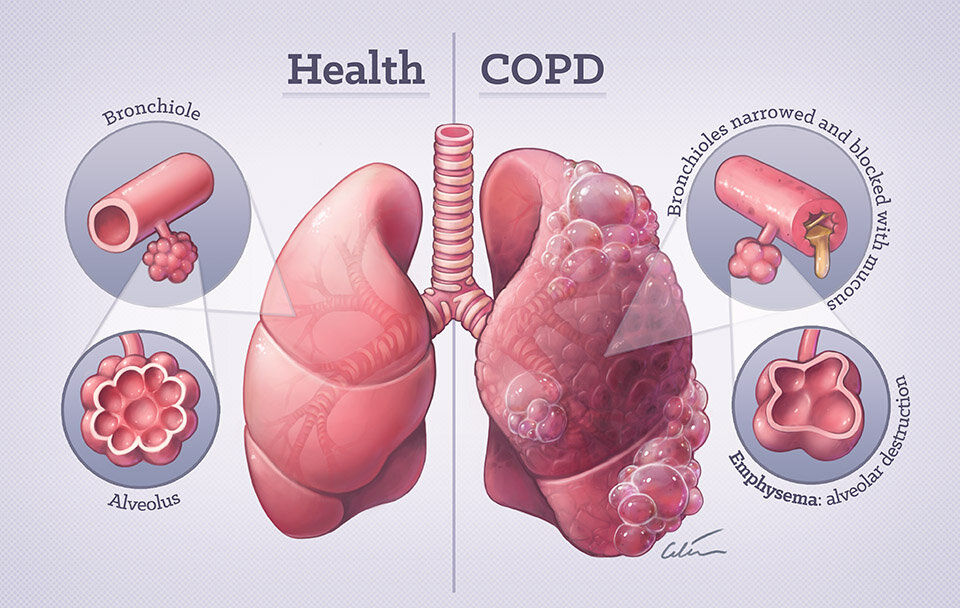
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. Symptoms include breathing difficulty, cough, mucus (sputum) production and wheezing. It’s caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. People with COPD are at increased risk of developing heart disease, lung cancer and a variety of other conditions.
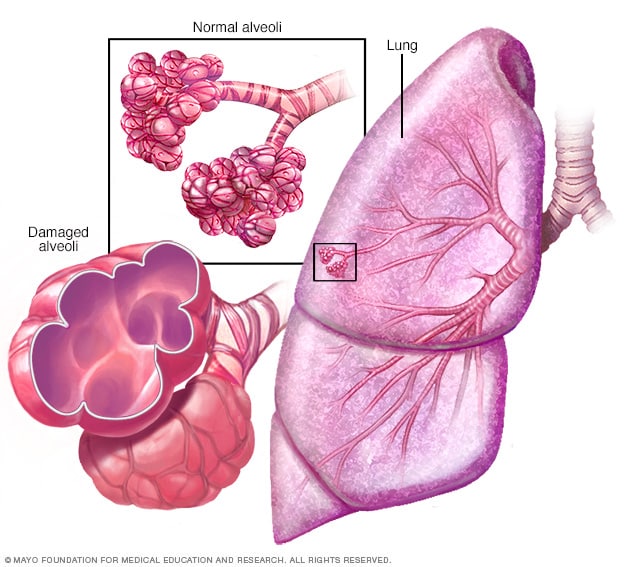
Emphysema is a condition in which the alveoli at the end of the smallest air passages (bronchioles) of the lungs are destroyed as a result of damaging exposure to cigarette smoke and other irritating gases and particulate matter.
COPD is treatable. With proper management, most people with COPD can achieve good symptom control and quality of life, as well as reduced risk of other associated conditions.
Symptoms of the Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease symptoms often don’t appear until significant lung damage has occurred, and they usually worsen over time, particularly if smoking exposure continues. For chronic bronchitis, the main symptom is a daily cough and mucus (sputum) production at least three months a year for two consecutive years.
Other signs and symptoms of the Chronic obstructive pulmonary disease may include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Having to clear your throat first thing in the morning, due to excess mucus in your lungs
- A chronic cough that may produce mucus (sputum) that may be clear, white, yellow or greenish
- The blueness of the lips or fingernail beds (cyanosis)
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet or legs
People with COPD are also likely to experience episodes called exacerbations, during which their symptoms become worse than usual day-to-day variation and persist for at least several days.
Causes of Chronic obstructive pulmonary disease
The main cause of COPD in developed countries is tobacco smoking. In the developing world, the Chronic obstructive pulmonary disease often occurs in people exposed to fumes from burning fuel for cooking and heating in poorly ventilated homes.
Only about 20 to 30 per cent of chronic smokers may develop clinically apparent COPD, although many smokers with long smoking histories may develop reduced lung function. Some smokers develop less common lung conditions. They may be misdiagnosed as having COPD until a more thorough evaluation is performed.
How your lungs are affected
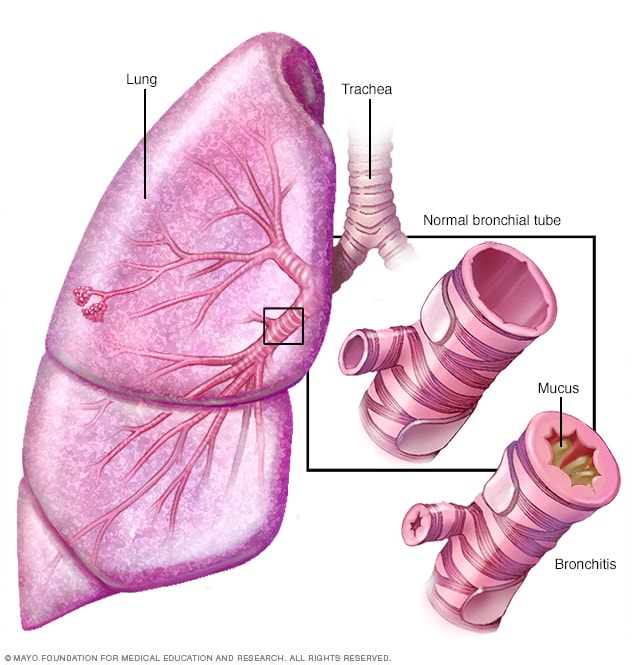
Air travels down your windpipe (trachea) and into your lungs through two large tubes (bronchi). Inside your lungs, these tubes divide many times — like the branches of a tree — into many smaller tubes (bronchioles) that end in clusters of tiny air sacs (alveoli).
The air sacs have very thin walls full of tiny blood vessels (capillaries). The oxygen in the air you inhale passes into these blood vessels and enters your bloodstream. At the same time, carbon dioxide — a gas that is a waste product of metabolism — is exhaled.
Your lungs rely on the natural elasticity of the bronchial tubes and air sacs to force air out of your body. The chronic obstructive pulmonary disease causes them to lose their elasticity and overexpand, which leaves some air trapped in your lungs when you exhale.
-
Emphysema
Causes of airway obstruction
Causes of airway obstruction include:
- Emphysema. This lung disease causes the destruction of the fragile walls and elastic fibres of the alveoli. Small airways collapse when you exhale, impairing airflow out of your lungs.
- Chronic bronchitis. In this condition, your bronchial tubes become inflamed and narrowed and your lungs produce more mucus, which can further block the narrowed tubes. You develop a chronic cough trying to clear your airways.
Cigarette smoke and other irritants
In the vast majority of cases, the lung damage that leads to COPD is caused by long-term cigarette smoking. But there are likely other factors at play in the development of COPD, such as a genetic susceptibility to the disease, because only about 20 to 30 per cent of smokers may develop COPD.
Other irritants can cause COPD, including cigar smoke, secondhand smoke, pipe smoke, air pollution and workplace exposure to dust, smoke or fumes.
Alpha-1-antitrypsin deficiency
In about 1 per cent of people with a Chronic obstructive pulmonary disease, the disease results from a genetic disorder that causes low levels of a protein called alpha-1-antitrypsin. Alpha-1-antitrypsin (AAT) is made in the liver and secreted into the bloodstream to help protect the lungs. Alpha-1-antitrypsin deficiency can affect the liver as well as the lungs. Damage to the lung can occur in infants and children, not only adults with long smoking histories.
For adults with COPD related to AAT deficiency, treatment options include those used for people with more-common types of COPD. In addition, some people can be treated by replacing the missing AAT protein, which may prevent further damage to the lungs.
Risk factors
Risk factors for COPD include:
- Exposure to tobacco smoke. The most significant risk factor for COPD is long-term cigarette smoking. The more years you smoke and the more packs you smoke, the greater your risk. Pipe smokers, cigar smokers and marijuana smokers also may be at risk, as well as people exposed to large amounts of secondhand smoke.
- People with asthma who smoke. The combination of asthma, a chronic inflammatory airway disease, and smoking increases the risk of COPD even more.
- Occupational exposure to dust and chemicals. Long-term exposure to chemical fumes, vapours and dust in the workplace can irritate and inflame your lungs.
- Exposure to fumes from burning fuel. In the developing world, people exposed to fumes from burning fuel for cooking and heating in poorly ventilated homes are at higher risk of developing COPD.
- Age. COPD develops slowly over years, so most people are at least 40 years old when symptoms begin.
- Genetics. The uncommon genetic disorder alpha-1-antitrypsin deficiency is the cause of some cases of COPD. Other genetic factors likely make certain smokers more susceptible to the disease.
Complications
The chronic obstructive pulmonary disease can cause many complications, including:
- Respiratory infections. People with COPD are more likely to catch colds, the flu and pneumonia. Any respiratory infection can make it much more difficult to breathe and could cause further damage to lung tissue. An annual flu vaccination and regular vaccination against pneumococcal pneumonia can prevent some infections.
- Heart problems. For reasons that aren’t fully understood, COPD can increase your risk of heart disease, including heart attack. Quitting smoking may reduce this risk.
- Lung cancer. People with COPD have a higher risk of developing lung cancer. Quitting smoking may reduce this risk.
- High blood pressure in lung arteries. COPD may cause high blood pressure in the arteries that bring blood to your lungs (pulmonary hypertension).
- Depression. Difficulty breathing can keep you from doing activities that you enjoy. And dealing with serious illness can contribute to the development of depression. Talk to your doctor if you feel sad or helpless or think that you may be experiencing depression.
Prevention
Unlike some diseases, COPD has a clear cause and a clear path of prevention. The majority of cases are directly related to cigarette smoking, and the best way to prevent COPD is to never smoke — or to stop smoking now.
If you’re a longtime smoker, these simple statements may not seem so simple, especially if you’ve tried quitting — once, twice or many times before. But keep trying to quit. It’s critical to find a tobacco cessation program that can help you quit for good. It’s your best chance for preventing damage to your lungs.
Occupational exposure to chemical fumes and dust is another risk factor for COPD. If you work with this type of lung irritant, talk to your supervisor about the best ways to protect yourself, such as using the respiratory protective equipment.
Diagnosis
The chronic obstructive pulmonary disease is commonly misdiagnosed — former smokers may sometimes be told they have COPD, when in reality they may have simple deconditioning or another less common lung condition. Likewise, many people who have COPD may not be diagnosed until the disease is advanced and interventions are less effective.
To diagnose your condition, your doctor will review your signs and symptoms, discuss your family and medical history, and discuss any exposure you’ve had to lung irritants — especially cigarette smoke. Your doctor may order several tests to diagnose your condition.
Tests may include:
- Lung (pulmonary) function tests. Pulmonary function tests measure the amount of air you can inhale and exhale, and if your lungs are delivering enough oxygen to your blood. Spirometry is the most common lung function test. During this test, you’ll be asked to blow into a large tube connected to a small machine called a spirometer. This machine measures how much air your lungs can hold and how fast you can blow the air out of your lungs. Spirometry can detect COPD even before you have symptoms of the disease. It can also be used to track the progression of a disease and to monitor how well treatment is working. Spirometry often includes measurement of the effect of bronchodilator administration. Other lung function tests include measurement of lung volumes, diffusing capacity and pulse oximetry.
- Chest X-ray. A chest X-ray can show emphysema, one of the main causes of COPD. An X-ray can also rule out other lung problems or heart failure.
- CT scan. A CT scan of your lungs can help detect emphysema and help determine if you might benefit from surgery for COPD. CT scans can also be used to screen for lung cancer.
- Arterial blood gas analysis. This blood test measures how well your lungs are bringing oxygen into your blood and removing carbon dioxide.
- Laboratory tests. Laboratory tests aren’t used to diagnose COPD, but they may be used to determine the cause of your symptoms or rule out other conditions. For example, laboratory tests may be used to determine if you have the genetic disorder alpha-1-antitrypsin (AAT) deficiency, which may be the cause of some cases of COPD. This test may be done if you have a family history of COPD and develop COPD at a young age, such as under age 45.
Treatment of Chronic obstructive pulmonary disease
A diagnosis of COPD is not the end of the world. Most people have mild forms of the disease for which little therapy is needed other than smoking cessation. Even for more advanced stages of a disease, effective therapy is available that can control symptoms, reduce your risk of complications and exacerbations, and improve your ability to lead an active life.
Smoking cessation
The most essential step in any treatment plan for COPD is to stop all smoking. It’s the only way to keep COPD from getting worse — which can eventually reduce your ability to breathe. But quitting smoking isn’t easy. And this task may seem particularly daunting if you’ve tried to quit and have been unsuccessful.
Talk to your doctor about nicotine replacement products and medications that might help, as well as how to handle relapses. Your doctor may also recommend a support group for people who want to quit smoking. It’s also a good idea to avoid secondhand smoke exposure whenever possible.
Medications
Doctors use several kinds of medications to treat the symptoms and complications of COPD. You may take some medications on a regular basis and others as needed.
Bronchodilators
These medications — which usually come in an inhaler — relax the muscles around your airways. This can help relieve coughing and shortness of breath and make breathing easier. Depending on the severity of your disease, you may need a short-acting bronchodilator before activities, a long-acting bronchodilator that you use every day or both.
Short-acting bronchodilators include albuterol (ProAir HFA, Ventolin HFA, others), levalbuterol (Xopenex HFA), and ipratropium (Atrovent). The long-acting bronchodilators include tiotropium (Spiriva), salmeterol (Serevent), formoterol (Foradil, Perforomist), arformoterol (Brovana), indacaterol (Arcapta) and aclidinium (Tudorza).
Inhaled steroids
Inhaled corticosteroid medications can reduce airway inflammation and help prevent exacerbations. Side effects may include bruising, oral infections and hoarseness. These medications are useful for people with frequent exacerbations of the Chronic obstructive pulmonary disease. Fluticasone (Flovent HFA, Flonase, others) and budesonide (Pulmicort Flexhaler, Uceris, others) are examples of inhaled steroids.
Combination inhalers
Some medications combine bronchodilators and inhaled steroids. Salmeterol and fluticasone (Advair) and formoterol and budesonide (Symbicort) are examples of combination inhalers.
Oral steroids
For people who have a moderate or severe acute exacerbation, short courses (for example, five days) of oral corticosteroids prevent further worsening of COPD. However, long-term use of these medications can have serious side effects, such as weight gain, diabetes, osteoporosis, cataracts and an increased risk of infection.
Phosphodiesterase-4 inhibitors
A new type of medication approved for people with severe COPD and symptoms of chronic bronchitis is roflumilast (Daliresp), a phosphodiesterase-4 inhibitor. This drug decreases airway inflammation and relaxes the airways. Common side effects include diarrhoea and weight loss.
Theophylline
This very inexpensive medication may help improve breathing and prevent exacerbations. Side effects may include nausea, headache, fast heartbeat and tremor. Side effects are dose-related, and low doses are recommended.
Antibiotics
Respiratory infections, such as acute bronchitis, pneumonia and influenza, can aggravate Chronic obstructive pulmonary disease symptoms. Antibiotics help treat acute exacerbations, but they aren’t generally recommended for prevention. However, a recent study shows that the antibiotic azithromycin prevents exacerbations, but it isn’t clear whether this is due to its antibiotic effect or its anti-inflammatory properties.
Lung therapies
Doctors often use these additional therapies for people with moderate or severe COPD:
- Oxygen therapy. If there isn’t enough oxygen in your blood, you may need supplemental oxygen. There are several devices to deliver oxygen to your lungs, including lightweight, portable units that you can take with you to run errands and get around town. Some people with COPD use oxygen only during activities or while sleeping. Others use oxygen all the time. Oxygen therapy can improve quality of life and is the only COPD therapy proven to extend life. Talk to your doctor about your needs and options.
- Pulmonary rehabilitation program. These programs generally combine education, exercise training, nutrition advice and counselling. You’ll work with a variety of specialists, who can tailor your rehabilitation program to meet your needs. Pulmonary rehabilitation may shorten hospitalizations, increase your ability to participate in everyday activities and improve your quality of life. Talk to your doctor about a referral to a program.
Managing exacerbations
Even with ongoing treatment, you may experience times when symptoms become worse for days or weeks. This is called an acute exacerbation, and it may lead to lung failure if you don’t receive prompt treatment.
Exacerbations may be caused by a respiratory infection, air pollution or other triggers of inflammation. Whatever the cause, it’s important to seek prompt medical help if you notice a sustained increase in coughing, a change in your mucus or if you have a harder time breathing.
When exacerbations occur, you may need additional medications (such as antibiotics, steroids or both), supplemental oxygen or treatment in the hospital. Once symptoms improve, your doctor will talk with you about measures to prevent future exacerbations, such as quitting smoking, taking inhaled steroids, long-acting bronchodilators or other medications, getting your annual flu vaccine, and avoiding air pollution whenever possible.
Surgery
Surgery is an option for some people with some forms of severe emphysema who aren’t helped sufficiently by medications alone. Surgical options include:
- Lung volume reduction surgery. In this surgery, your surgeon removes small wedges of damaged lung tissue from the upper lungs. This creates extra space in your chest cavity so that the remaining healthier lung tissue can expand and the diaphragm can work more efficiently. In some people, this surgery can improve quality of life and prolong survival.
- Lung transplant. Lung transplantation may be an option for certain people who meet specific criteria. Transplantation can improve your ability to breathe and to be active. However, it’s a major operation that has significant risks, such as organ rejection, and it’s necessary to take lifelong immune-suppressing medications.
- Bullectomy. Large air spaces (bullae) form in the lungs when the walls of the air sacs are destroyed. These bullae can become very large and cause breathing problems. In a bullectomy, doctors remove bullae from the lungs to help improve airflow.
Clinical trials
Lifestyle and home remedies
If you have COPD, you can take steps to feel better and slow the damage to your lungs:
- Control your breathing. Talk to your doctor or respiratory therapist about techniques for breathing more efficiently throughout the day. Also be sure to discuss breathing positions and relaxation techniques that you can use when you’re short of breath.
- Clear your airways. With COPD, mucus tends to collect in your air passages and can be difficult to clear. Controlled coughing, drinking plenty of water and using a humidifier may help.
- Exercise regularly. It may seem difficult to exercise when you have trouble breathing, but regular exercise can improve your overall strength and endurance and strengthen your respiratory muscles. Discuss with your doctor which activities are appropriate for you.
- Eat healthy foods. A healthy diet can help you maintain your strength. If you’re underweight, your doctor may recommend nutritional supplements. If you’re overweight, losing weight can significantly help your breathing, especially during times of exertion.
- Avoid smoke and air pollution. In addition to quitting smoking, it’s important to avoid places where others smoke. Secondhand smoke may contribute to further lung damage. Other types of air pollution also can irritate your lungs.
- See your doctor regularly. Stick to your appointment schedule, even if you’re feeling fine. It’s important to steadily monitor your lung function. And be sure to get your annual flu vaccine in the fall to help prevent infections that can worsen your COPD. Ask your doctor when you need the pneumococcal vaccine. Let your doctor know if you have worsening symptoms or you notice signs of infection.
Coping and support
Living with COPD can be a challenge — especially as it becomes harder to catch your breath. You may have to give up some activities you previously enjoyed. Your family and friends may have difficulty adjusting to some of the changes.
It can help to share your fears and feelings with your family, friends and doctor. You may also want to consider joining a support group for people with COPD. And you may benefit from counselling or medication if you feel depressed or overwhelmed.
Preparing for your appointment
If your primary care doctor suspects that you have COPD, you’ll likely be referred to a pulmonologist — a doctor who specializes in lung disorders.
What you can do
Before your appointment, you might want to write a list of answers to the following questions:
- What symptoms are you experiencing? When did they start?
- What makes your symptoms worse? Better?
- Does anyone in your family have COPD?
- Have you had any treatment for COPD? If so, what was it and did it help?
- Have you ever taken beta blockers for your high blood pressure or heart?
- Are you being treated for any other medical conditions?
- What medications and supplements do you take regularly?
You might want to have a friend or family member accompany you to your appointment. Often, two sets of ears are better than one when you’re learning about a complicated medical problem, such as COPD. Take notes if this helps.
What to expect from your doctor
Your doctor may ask some of the following questions:
- How long have you had a cough?
- Do you get short of breath easily?
- Have you noticed any wheezing when you breathe?
- Do you or have you ever smoked cigarettes?
- Would you like help in quitting?
Treatment for COPD
Treatment can ease symptoms, prevent complications, and generally slow disease progression. Your healthcare team may include a lung specialist (pulmonologist) and physical and respiratory therapists.
Medication
Bronchodilators are medications that help relax the muscles of the airways so you can breathe easier. They’re usually taken through an inhaler. Glucocorticosteroids can be added to reduce inflammation in the airways.
To lower risk of other respiratory infections, ask your doctor if you should get a yearly flu shot, pneumococcal vaccine, and a tetanus booster that includes protection from pertussis or whooping cough.
Oxygen therapy
If your blood oxygen levels are low, you can receive oxygen through a mask or nasal prongs to help you breathe better. A portable unit can make it easier to get around.
Surgery
Surgery is reserved for severe COPD or when other treatments have failed, which is more likely when you have emphysema. One type of surgery is called bullectomy. That’s when surgeons remove large air sacs (bullae) from the lungs. Another is lung volume reduction surgery, which removes damaged lung tissue.
Lung transplant is an option in some cases.
Lifestyle changes
Certain lifestyle changes may also help alleviate your symptoms or provide relief.
These include:
- If you smoke, quit. Your doctor can recommend appropriate products or support services.
- Whenever possible, avoid secondhand smoke and chemical fumes.
- Get the nutrition your body needs. Work with your doctor or dietician to create a healthy eating plan.
- Talk to your doctor about how much exercise is safe for you.
Medications can reduce symptoms and cut down on flare-ups. It may take a bit of trial and error to find the medication and dosage that works best for you. These are some of your options:
Bronchodilators
Medicines called bronchodilators to help loosen tight muscles around your airways. They are typically taken through an inhaler or nebulizer.
Short-acting bronchodilators last from four to six hours. You only use them when you need them. For ongoing symptoms, there are long-acting versions you can use every day. They last about 12 hours.
Some bronchodilators are beta-agonists. They work by relaxing tightened muscles around the airways. Some are anticholinergics. They prevent muscle tightening and clear mucus from the lungs. Anticholinergics can also be taken with a nebulizer.
Corticosteroids
Sometimes bronchodilators are combined with inhaled glucocorticosteroids. Using the two together can reduce inflammation in the airways and lower mucus production. Corticosteroids are also available in pill form.
Phosphodiesterase-4 inhibitors
This newer medication in pill form reduces inflammation and changes mucus production. It’s generally prescribed for severe COPD.
Theophylline
This medicine eases chest tightness and shortness of breath. It may help prevent flare-ups. It’s available in pill form.
Antibiotics and antivirals
Antibiotics or antivirals may be prescribed when you develop respiratory infections.
Vaccines
COPD increases your risk of other respiratory problems. For that reason, your doctor might recommend that you get a yearly flu shot, the pneumococcal vaccine, or the whooping cough vaccine.
DIET
There’s no specific diet for COPD, but a healthy diet is important for maintaining overall health. The stronger you are, the abler you’ll be to prevent complications and other health problems.
Choose a variety of nutritious foods from these groups:
- vegetables
- fruits
- grains
- protein
- dairy
Drink plenty of fluids. Drinking six to eight 8-ounce glasses of noncaffeinated liquids a day can help keep mucus on the thin side. This may make the mucus easier to clear out. Limit caffeinated beverages because they can interfere with medications and increase water loss. If you have heart problems, you may need to drink less, so talk to your doctor.
Go easy on the salt. It retains water, which can strain to breathe.
Weight matters. It takes more energy to breathe when you have COPD, so you might need to take in more calories. If you’re overweight, your lungs and heart may have to work harder. If you’re underweight or frail, even basic body maintenance can become difficult. Overall, having COPD weakens your immune system and decreases your ability to fight off infection.
A full stomach makes it harder for your lungs to expand, leaving you short of breath. If that happens, try these remedies:
- Clear your airways about an hour before a meal.
- Swap three meals a day for five or six smaller meals.
- Save fluids until the end so you feel less full during the meal.
COPD requires lifelong disease management. That means following the advice of your healthcare team. There’s a lot you can do on your own, too.
Remember, your lungs are weakened. You’ll want to avoid anything that might overtax them or cause a flare-up.
Number one on the list of things to avoid is smoking. If you’re having trouble quitting, talk to your doctor about smoking cessation programs. Try not to be around secondhand smoke, chemical fumes, air pollution, and dust.
A little exercise each day can help you stay strong. Talk to your doctor about how much exercise is good for you.
Maintain a diet of nutritious foods. Avoid highly processed foods that are loaded with calories and salt but lack nutrients.
If you have other chronic diseases along with COPD, it is important to manage those as well, particularly diabetes and heart disease.
Clear the clutter and streamline your home so that it takes less energy to clean and do other household tasks. If you have advanced COPD, get help with daily chores.
Be prepared. Carry your emergency contact information with you and post it on your refrigerator. Include information about what medications you take, as well as the doses. Program emergency numbers into your phone.
It can be a relief to talk to others who understand. Consider joining a support group. The COPD Foundation provides a comprehensive list of organizations and resources for people living with COPD.
One measure of COPD disease is by stage. The stages are:
Stage 0 – At risk: Symptoms include coughing and noticeable mucus. You don’t actually have COPD, so treatment isn’t necessarily needed. But do heed the warning. If you smoke, stop now. It would be wise to reassess your diet and exercise routines to improve overall health. Once you have COPD, it’s not reversible or curable.
Stage 1 – Mild: At this stage, some people still don’t notice symptoms, which may include a chronic cough and increased mucus production. If you visit a doctor at this point, chances are you’ll start using a bronchodilator as needed.
Stage 2 – Moderate: Symptoms are becoming more noticeable. In addition to a cough and mucus, you may start to experience shortness of breath. You may need a long-acting bronchodilator.
Stage 3 – Severe: Symptoms become more frequent and you may have occasional flare-ups of severe symptoms. You might find that it’s difficult to function normally. Your doctor may recommend corticosteroids, other medications, or oxygen therapy.
Stage 4 – Very severe: Symptoms are progressing and it’s harder to complete everyday tasks. Flare-ups can be life-threatening. You may be a candidate for surgical treatment.
As the disease progresses, you’re more susceptible to complications, such as:
- respiratory infections, including colds, flu, and pneumonia
- heart problems
- high blood pressure in lung arteries
- lung cancer
- depression
All around the world, COPD and lung cancer are major health problems. These two diseases are linked in a number of ways.
COPD and lung cancer have several common risk factors. Smoking is the number one risk factor for both diseases. Both are more likely if you breathe secondhand smoke, or are exposed to chemicals or other fumes in the workplace.
There may be a genetic predisposition to developing both diseases. Also, the risk of developing either COPD or lung cancer increase with age.
Between 40 and 70 per cent of people with lung cancer also have COPD. 2009 study concluded that COPD is, indeed, a risk factor for lung cancer.
A 2015 study suggests they may actually be different aspects of the same disease, and that COPD could be a driving factor in lung cancer.
In some cases, people don’t learn they have COPD until they’re diagnosed with lung cancer.
Of course, having a Chronic obstructive pulmonary disease doesn’t necessarily mean you’ll get lung cancer. You do have a higher risk though. That’s another reason why, if you smoke, quitting is a good idea.
Worldwide, about 65 million people have moderate to severe COPD. About 12 million adults in the United States have a diagnosis of COPD. It’s estimated that 12 million more have the disease, but don’t know it yet.
Most people with the Chronic obstructive pulmonary disease are 40 years of age or older.
The majority of people with COPD are smokers or former smokers. Smoking is the most important risk factor that can be changed. Between 20 and 30 per cent of chronic smokers develop COPD.
Between 10 and 20 per cent of people with COPD have never smoked. In up to 5 per cent of people with COPD, the cause is a genetic disorder involving low levels of a protein called alpha-1-antitrypsin.
The chronic obstructive pulmonary disease is a leading cause of hospitalizations in industrialized countries. In the United States, COPD is responsible for over 700,00 hospital admissions per year and over 1.5 million emergency department visits. Among people with lung cancer, between 40 and 70 per cent also have COPD.
About 120,000 people die from COPD each year in the United States. It’s the third leading cause of death in the United States. More women than men die from COPD each year.
It is projected that the number of COPD cases will increase by more than 150 per cent from 2010 to 2030. Much of that can be attributed to an ageing population.
The chronic obstructive pulmonary disease tends to progress slowly. You may not even know you have it during the early stages.
Once you have a diagnosis, you’ll need to start seeing your doctor on a regular basis. You’ll also have to take steps to manage your condition and make the appropriate changes to your daily life.
Early symptoms can be managed, and certain lifestyle choices can help you maintain a good quality of life for some time.
As the disease progresses, symptoms can become increasingly limiting.
In severe stages of the Chronic obstructive pulmonary disease, you may not be able to care for yourself without assistance. You’re at increased risk of developing other respiratory infections, heart problems, and lung cancer. You may also be at risk of depression.
The chronic obstructive pulmonary disease generally reduces life expectancy, though the outlook varies considerably from person to person. People with COPD who never smoked may have a modest reduction in life expectancy, while former and current smokers are likely to have a larger reduction.
Besides smoking, your outlook depends on how well you respond to treatment and whether you can avoid serious complications. Your doctor is in the best position to evaluate your overall health and give you an idea of what to expect.








Leave a Reply